In just a few months, COVID-19 has transformed the practice of emergency medicine. As a way to better understand the impact COVID-19 has had on fluid resuscitation in emergent care of patients in shock, we recently conducted a brief online survey. A total of eighteen (18) respondents provided feedback ranking the considerations in fluid resuscitation and fluid delivery device benefits. Respondents consisted of emergency room nurses, ICU nurses and clinical educators. Our key takeaway is that nurses continue see rapid delivery of a controlled fluid bolus as a priority for patient management, along with the desire for speed in patient stabilization.
Our survey results revealed that the highest need is to stabilize a patient quickly in order to make treatment decisions. Secondly, and perhaps more influenced by COVID-19, is the need to precisely control fluid administration to restore perfusion and avoid fluid overload. Early data has indicated that it is not uncommon for COVID-19 patients to present with pulmonary or cardiac complications. Although a recent study1 demonstrated that shock patients in heart or renal failure are no more likely to require ventilation than shock patients without such conditions, we know that excess fluids can be harmful, and thus it aligns that emergent care of COVID-19 patients would involve heightened fluid volume monitoring and response.
Additional criteria included minimizing trips in and out of the room/PPE changes, accelerating disposition time, and minimizing use of equipment requiring disinfection. Interestingly, we expected infection control to rank higher in this survey, as our anecdotal feedback has indicated a new emphasis on minimizing donning/doffing PPE and cleaning of reusable equipment. Figure 1 below indicates the entire spectrum of response rankings.
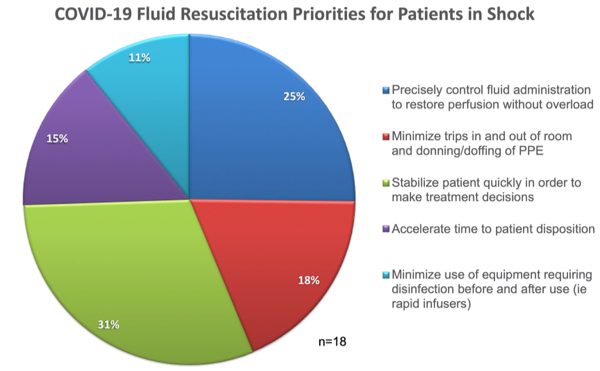
Figure 1. Fluid Resuscitation Priorities Ranked by Nurses.
The survey also polled respondents on the desired benefits in a fluid delivery device during this time of COVID-19. The answer came across loud and clear…speed and simplicity. The top ranked product need was fast, easy product set-up, closely followed by faster completion of first bolus. These answers highlight that in the moment of managing a crashing patient, nurses perceive that time is of the essence. Additional criteria included user ability to titrate fluids, portability and disposability/single-use. Figure 2 shows the full breakdown of device benefits ranking. Again, we were a little surprised to see disposability/single-use ranked last, but again, this is a very small dataset and it didn’t include any nurse or quality managers.
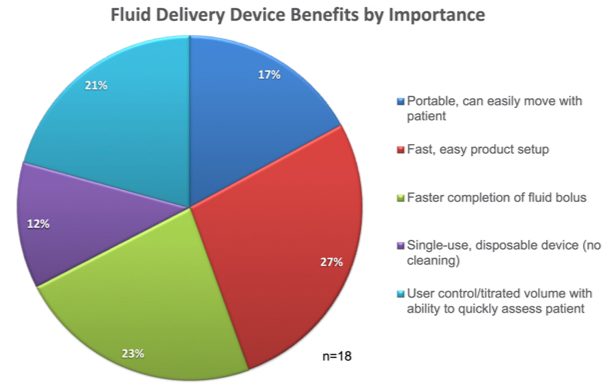
Figure 2. Fluid Delivery Device Benefits Ranked by Importance
Obviously, we need to be careful to not draw firm conclusions from such a small dataset. However, it seems clear that in spite of, or perhaps because of COVID-19, nurses are seeking the ability to quickly address shock with fluids while maintaining control over volume. A few respondents provided comments focused on the desire to approach COVID-19 patients more conservatively with concern of fluid overload affecting pulmonary function. Comments reflected a change in addressing COVID-19 patients with shock with vasopressors being used earlier in the resuscitation process.
If you’d like to provide feedback on these results or your own experience, we would love to hear from you. You can reach us here.
Khan RA, Khan NA, Bauer SR, et al. Association Between Volume of Fluid Resuscitation and Intubation in High-Risk Patients With Sepsis, Heart Failure, End-Stage Renal Disease, and Cirrhosis. Chest. 2020;157(2):286-292. doi:10.1016/j.chest.2019.09.029.

