
Sepsis is the costliest condition treated in US hospitals and is responsible for one in three inpatient deaths.1,2 Since publication of the Early Goal Directed Therapy (EGDT) trial in 2001, worldwide attention has been focused on improving sepsis care through the adoption of sepsis protocols, which have been a major factor in improving patient outcomes. Debate has continued, however, about the optimal timing and volume of fluid resuscitation for severe sepsis and septic shock.3,4,5
A recent meta-analysis by Ward, et al, in the Journal of Intensive Care Medicine examines this question by pooling data from retrospective studies evaluating the role of early fluid resuscitation in sepsis (figure 1).6Among three hospital-based studies analyzed, a survival benefit was seen with earlier fluid initiation among patients all patients. When two EMS studies were included, the same effect was observed, but only among patients with hypotension. These data provide further support of the effectiveness of early fluid resuscitation guidelines, particularly for patients with septic shock and hypotension.
Figure 1
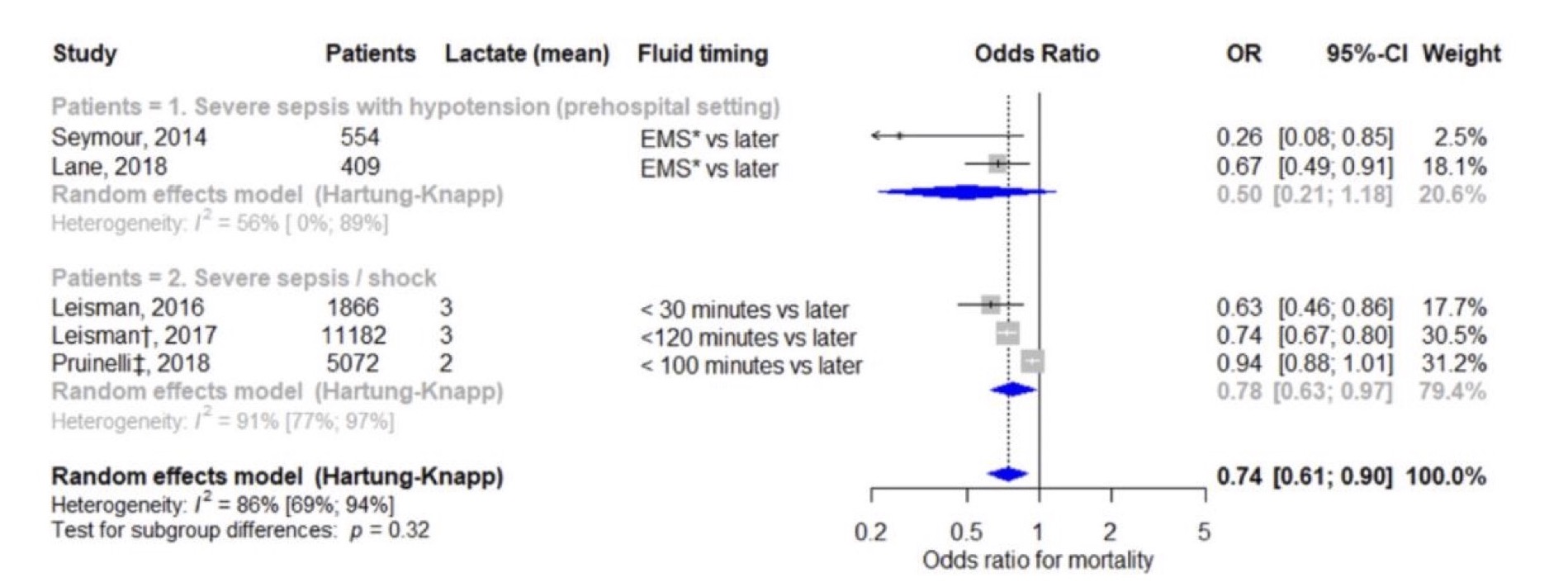
While excess fluid accumulation in the ICU can lead to adverse outcomes in patients with sepsis, a thoughtful initial approach to fluid resuscitation can reverse shock earlier and reduce total fluid requirements. As Ward points out in his recent editorial on the Surviving Sepsis Campaign bundle, the controversy around fluid resuscitation guidelines has often resulted from a focus of the late harms of volume overload, obscuring the evidence of early shock reversal with fluid resuscitation delivered rapidly and titrated to patient response.7 The meta-analysis by Ward reminds us that minutes do matter in sepsis and demonstrates that earlier fluid resuscitation is particularly important for patients with hypotension.
1. Lelubre C, et al. Mechanisms and treatment of organ failure in sepsis. Nat Rev Nephrol 14, 417–427 (2018) doi:10.1038/s41581-018-0005-.
2. Liang L (AHRQ), Moore B (IBM Watson Health), Soni A (AHRQ). National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2017. HCUP Statistical Brief #261. Month 2020. Agency for Healthcare Research and Quality, Rockville, MD. www.hcup-us.ahrq.gov/reports/statbriefs/sb261-Most-Expensive-Hospital-Conditions-2017.pdf
3. Rivers E., Nguyen B., Havstad S., Ressler J., Muzzin A., Knoblich B. et al. (2001). Early goal-directed therapy in the treatment of severe sepsis and septic shock. New England Journal of Emergency Medicine. 345(19):1368-77.
4. Levy, Mitchell M. MD, MCCM1; Evans, Laura E. MD, MSc, FCCM2; Rhodes, Andrew MBBS, FRCA, FRCP, FFICM, MD (res)3 The Surviving Sepsis Campaign Bundle: 2018 Update, Critical Care Medicine: June 2018 – Volume 46 – Issue 6 – p 997-1000 doi: 10.1097/CCM.0000000000003119.
5. Dhooria S., & Agarwal R. (2015). Early goal-directed therapy versus early and goal-directed therapy for severe sepsis and septic shock: time to rationalize. Lung India; 325):521-3.
6. Ward MA, Kuttab HI, Tuck N, Taleb A, Okut H, Badgett RG. The Effect of Fluid Initiation Timing on Sepsis Mortality: A Meta-Analysis. J Intensive Care Med. 2022;37(11):1504-1511.
7. Ward MA. The American College of Emergency Physicians Policy Statement on Sepsis-based Fluid Resuscitation Thirsts for Supporting Evidence and Balance. Ann Emerg Med. 2022;79(3):318-319.

