
Emergency departments (EDs) must be ready for anything. In critical situations, every minute matters. So does having the right equipment. Sadly, data from the Wall Street Journal shows that just 14% of non-pediatric specialized facilities are certified and prepared when a pediatric patient arrives.1
Lax regulations, or a total absence of verification programs in most states, mean that hospitals aren’t mandated to maintain a high level of pediatric readiness. The result is higher mortality rates and avoidable patient deaths. Reversing this narrative and ensuring every U.S. hospital is fully prepared to treat the full range of pediatric emergencies is a crucial need that requires urgent action.
Assessing the Pediatric Readiness Landscape in U.S. Emergency Departments
In the fast-paced world of emergency medicine, there are endless scales and scores for quickly assessing both the patient and the facility around them. Nationwide, children represent 25% of all ED visits.2 Yet, only 23 states have a pediatric readiness verification program.1 Though two more plan to launch one this year, 50% is a massive failure of accountability within the healthcare system.
The National Pediatric Readiness Project Assessment defines a “high” level of pediatric readiness as scoring above 87 points on its specially developed 100-point scale.3 Adult EDs meeting these criteria witness a 76% lower mortality rate in ill children and a 60% lower mortality rate in injured children.3 While research is ongoing, experts believe a similar impact will be revealed in EMS settings.
However, according to Becker’s Hospital Review, just five states are deemed 50% or more pediatric ready—the percentage of hospitals with preparations certified by the state to treat pediatric emergencies. Those states are Delaware, Utah, Illinois, New Jersey, and Tennessee.4 Only the latter three have a mandatory preparedness program, while the rest are voluntary. The same data reveals that 34 states fall at 10% readiness or below (Figure 1).4
Figure 1
Pediatric-ready Hospitals by State
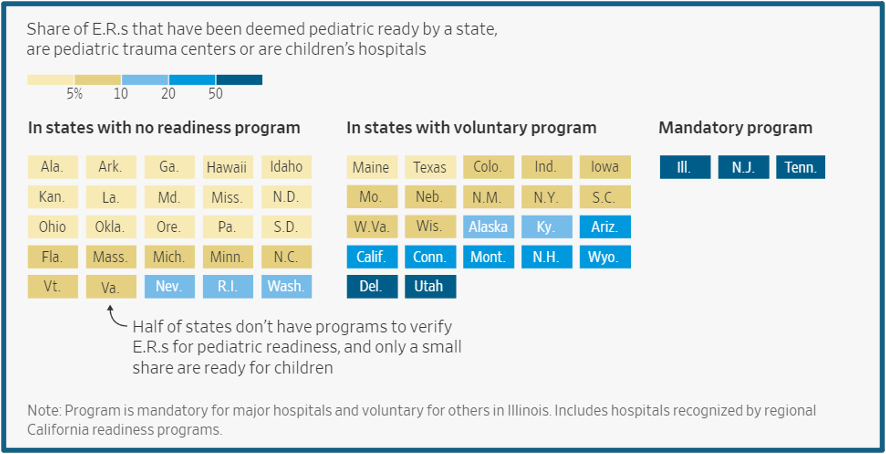
Evans et al. “Pediatric-ready hospitals.” Wall Street Journal, October 1, 2023.
The Fatal Consequences of Unpreparedness
As the common healthcare academia saying goes, children are not little adults. The drastic size variation within the pediatric population is one factor. A six-month-old infant requires far smaller equipment than a 15-year-old student-athlete. Perhaps more importantly, though, are the psychological and physiological differences between pediatric patients and adults. For instance, a 6kg infant who loses just 180 mLs of fluid volume can enter decompensated hypotensive shock.6 As a result, providers must be knowledgeable and prepared to respond promptly with effective interventions. When they are not, the consequences are clear.
According to a 2023 JAMA article summarizing a study of nearly 800,000 children cared for across 983 EDs between 2012 and 2017, an estimated 1,442 deaths could have been prevented if every ED had a high level of pediatric readiness (Figure 2).7 Meanwhile, a CBS News segment citing a study from Pediatrics found that children are four times more likely to die in hospital emergency rooms with the lowest pediatric readiness scores.8
Figure 2
Adjusted Time to Death for Injured and Medical Children, by Emergency Department (ED) Pediatric Readiness
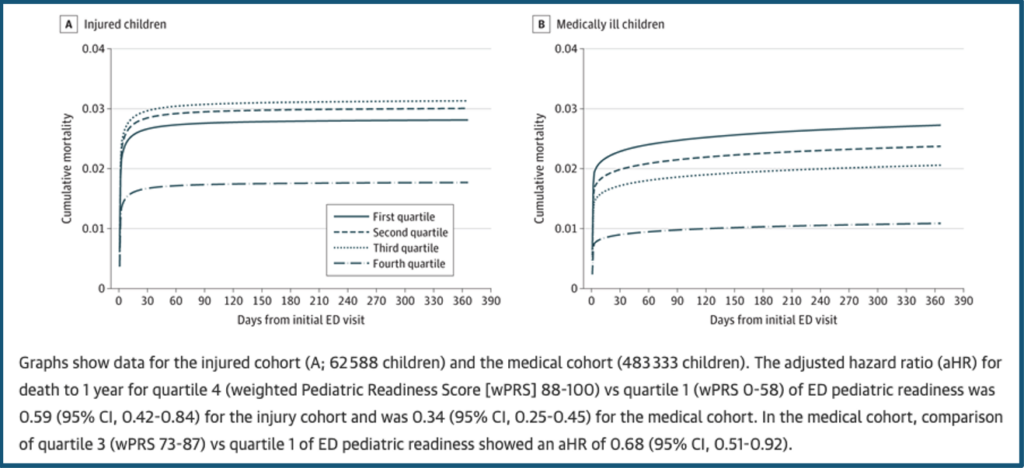
2 Newgard CD, Lin A, Malveua S, et al. Emergency Department Pediatric Readiness and Short-term and Long-term Mortality Among Children Receiving Emergency Care. JAMA Netw Open.2023;6(1):ee2250941.doi:10.1001/jamanetworkiopen.2022.50941
Peregrine Health Services identified that five out of six children (83%) who need emergency care first present to an ED that is not a specialized pediatric hospital.5 Given these numbers, an enormous number of children receive care each year in facilities where they do not have the best chance of survival.3,7,8
The Path Forward: Advocating for Pediatric Readiness
Current evidence should encourage a commitment by all emergency departments to improve pediatric readiness. Doing so acknowledges the unique needs of our youngest patients and the specialized attention and equipment needed to care for them in emergent situations.
LifeFlow stands ready to be a partner in the campaign for pediatric readiness and is uniquely positioned to address one of the most common challenges in pediatric ED visits: rapid blood and fluid administration. Treating shock, dehydration, and severe blood loss relies on quickly replenishing blood or fluid volume.6 The handheld LifeFlow PLUS rapid infuser is easy to set up and can be operated one-handed by a single provider to infuse fluids or blood products in a controlled manner. Notably, the device’s patented Force Reducer smooths pulsatile flow, enabling rapid fluid resuscitation through small-bore IV catheters faster than other commonly used techniques like push-pull, electronic IV pumps, and pressure bags.9 LifeFlow also reduces the risk of infections and related complications by ensuring the provider never touches the syringe plunger during administration.9
As noted by Simone Greenberg, RN, BSN, CPEN of Joe DiMaggio Children’s Hospital, “Massive transfusion protocols are always stressful, particularly when it’s a pediatric case. Using LifeFlow in our pediatric traumas has helped us initiate the resuscitation quickly and simplify the administration of blood, which is critical for stabilizing the patient prior to transfer to the OR.”
Every step towards improved pediatric readiness is a step towards a future where the emergency care landscape is truly ready for anything. The goal is simple: saving lives. The National Pediatric Readiness Project (NPRP) aims to ensure every emergency department (ED) has the resources, competencies, and policies needed for high-quality, equitable pediatric emergency care.
To learn more about the National Pediatric Readiness Project and discover resources to help improve readiness, visit the EMSC Innovation and Improvement Center at: https://emscimprovement.center/domains/pediatric-readiness-project/.
- https://www.wsj.com/health/healthcare/emergency-rooms-hospitals-kids-1c41a8a8?mod=article_inline
- https://nap.nationalacademies.org/catalog/11655/emergency-care-for-children-growing-pains
- https://emscimprovement.center/domains/pediatric-readiness-project/
- https://www.beckershospitalreview.com/rankings-and-ratings/best-worst-states-for-ed-pediatric-preparedness.html?utm_medium=email&utm_content=newsletter
- https://peregrinehs.com/blog/a-concise-guide-to-complying-with-acs-standard-5-10/
- https://410medical.com/2019/10/01/when-minutes-matter-treating-pediatric-hypovolemic-shock-part-1/#:~:text=Children%20are%20known%20for%20their,compensated%20shock%20longer%20than%20adults.&text=Decompensated%20shock%20occurs%20after%20approximately%2030%25%20loss%20of%20volume.
- https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2800400
- https://www.cbsnews.com/video/how-pediatric-readiness-saves-lives-in-emergency-rooms/
- https://410medical.com/about/how-it-works/

