Prolonged shock can lead to poor perfusion, increasing the risk of organ failure and death. In June Frontiers in Medicine published a review article highlighting the increasing evidence supporting the use of a peripheral perfusion marker to guide shock treatment, diagnosis and prognosis.1 Patients in shock have varying degrees of shock progression as well as diverse needs for fluid resuscitation. In order to avoid the possible dangers of under or over fluid resuscitating, a fast, reliable marker is needed. As we highlighted in a previous Recent News, the ANDROMEDA-SHOCK trial showed using Capillary Refill Time (CRT) was a superior method than serum lactate as a guide for fluid resuscitation. The Frontiers in Medicine review article offers a more detailed physiological explanation as to why CRT may be a great indicator in shock.
Shock is defined as a state in which blood circulation is not able to deliver sufficient oxygen to match the demand of tissues.2 Skin perfusion is used mainly for thermoregulation and is controlled by the sympathetic system (not under metabolic control).3 The body’s reaction to hypotension is vasoconstriction by the sympathetic system, thereby reducing blood flow to the skin.4 Autoregulation then steps in to allow for organ blood flow, but the skin is mostly unaffected by autoregulation and decreased flow to the skin persists until the sympathetic response is no longer triggered.5
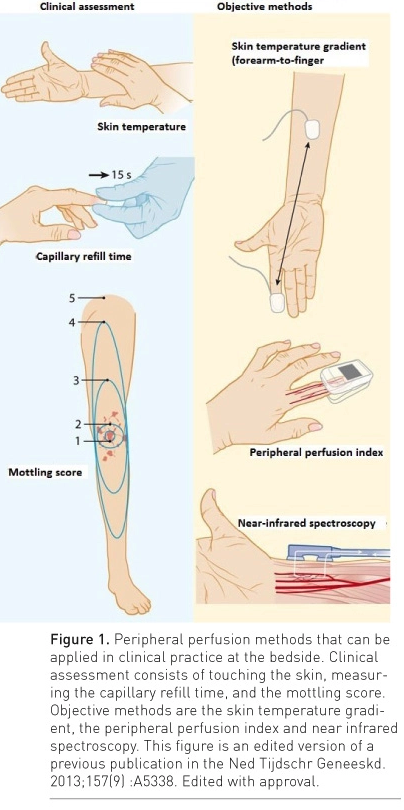
Figure from: https://healthmanagement.org/c/icu/issuearticle/monitoring-peripheral-circulation
CRT as well as skin temperature difference are related to severity and outcome in shock. 1,6,7,8,9-11 These parameters respond quickly to restoration of blood flow to tissues and fluid resuscitation can be shortened in patients with normal peripheral perfusion. In addition to the ANDROMEDA-SHOCK results showing an advantage to CRT over serum lactate, Brunauer et al. showed abdominal organ perfusion correlates with CRT when patients are in septic shock. 12
In summary, the authors of the Frontiers in Medicine review propose that CRT is a good indicator for tissue perfusion in septic shock patients and that it can be used to determine the treatment track (restrictive vs liberal fluid resuscitation) optimal for each patient. In addition, the authors suggest that CRT changes after an intervention such as fluid resuscitation correlate to abdominal organ perfusion and subsequently patient outcome. Viewed together, this review and paper by Kattan et al reviewed previously make a compelling case for broad use of CRT as a tool for guiding fluid resuscitation in patients with hypotension and shock. How do you measure perfusion? Contact us to share your approach.
- Bakker J, Hernandez G. Can Peripheral Skin Perfusion Be Used to Assess Organ Perfusion and Guide Resuscitation Interventions?. Front Med (Lausanne). 2020;7:291. Published 2020 Jun 23. doi:10.3389/fmed.2020.00291
- Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, et al. Consensus on circulatory shock and hemodynamic monitoring. Task force of the european society of intensive care medicine. Intensive Care Med. (2014) 40:1795–815. doi: 10.1007/s00134-014-3525-z
- Charkoudian N. Skin blood flow in adult human thermoregulation: how it works, when it does not, and why. Mayo Clin Proc. (2003) 78:603–12. doi: 10.4065/78.5.603
- Clifford PS. Local control of blood flow. Adv Physiol Educ. (2011) 35:5–15. doi: 10.1152/advan.00074.2010
- Jones RD, Berne RM. Intrinsic regulation of skeletal muscle blood flow. Circ Res. (1964) 14:126–38. doi: 10.1161/01.RES.14.2.126
- Champion HR, Sacco WJ, Carnazzo AJ, Copes W, Fouty WJ. Trauma score. Crit Care Med. (1981) 9:672–6. doi: 10.1097/00003246-198109000-00015
- van Genderen ME, van Bommel J, Lima A. Monitoring peripheral perfusion in critically ill patients at the bedside. Curr Opin Crit Care. (2012) 18:273–9. doi: 10.1097/MCC.0b013e3283533924
- Lara B, Enberg L, Ortega M, Leon P, Kripper C, Aguilera P, et al. Capillary refill time during fluid resuscitation in patients with sepsis-related hyperlactatemia at the emergency department is related to mortality. PLoS ONE. (2017) 12:e0188548. doi: 10.1371/journal.pone.0188548
- Lima A, van Bommel J, Jansen TC, Ince C, Bakker J. Low tissue oxygen saturation at the end of early goal-directed therapy is associated with worse outcome in critically ill patients. Critical Care. (2009) 13:S13. doi: 10.1186/cc8011
- Lima A, Jansen TC, Van Bommel J, Ince C, Bakker J. The prognostic value of the subjective assessment of peripheral perfusion in critically ill patients. Crit Care Med. (2009) 37:934–938. doi: 10.1097/CCM.0b013e31819869db
- Alegria L, Vera M, Dreyse J, Castro R, Carpio D, Henriquez C, et al. A hypoperfusion context may aid to interpret hyperlactatemia in sepsis-3 septic shock patients: a proof-of-concept study. Ann Intensive Care. (2017) 7:29. doi: 10.1186/s13613-017-0253-x
- Brunauer A, Kokofer A, Bataar O, Gradwohl-Matis I, Dankl D, Bakker J, et al. Changes in peripheral perfusion relate to visceral organ perfusion in early septic shock: A pilot study. J Crit Care. (2016) 35:105–9. doi: 10.1016/j.jcrc.2016.05.007

