
A 58 year-old hypotensive woman is transferred to your ICU from the ED with urosepsis. By all measures of fluid status and predictors of fluid responsiveness, the patient desperately needs more fluids. Recognizing that every minute that the patient remains hypotensive corresponds with increasing chance of end organ dysfunction and mortality (the dangers of passive resuscitation) the physician on call orders 2L of IV fluid and verbally instructs you to give the fluid as quickly as possible. As you consider the available options for delivering the fluid (gravity flow, infusion pump, pressure bag, rapid infuser) you reach for the pressure bag set up. What other thoughts are entering your mind as you proceed with setting up the pressure bag?
- How quickly can I set this up?
- How many times will I need to re-inflate the bag to maintain pressure?
- The patient only has a 20 gauge catheter, is using pressure bag really going to help?
- Will the pressure bag increase the risk of air embolism?
As you wrestle with these questions, you continue with the pressure bag set up because the rapid infuser is even more cumbersome and, in reality, you don’t have a ton of experience with that machine. You believe that the pressure bag will at least be faster than gravity flow and infusion pumps. However, you can’t help but wonder if this is really the best delivery method that we have, particularly for this hypotensive patient in shock.
If these thoughts are circling in your mind every time you reach for a pressure bag, you aren’t alone. A recent survey completed by over 50 nurses at the Emergency Nurses Association Annual Conference 2018 all agreed that hypotension is a medical emergency and that rapid fluid resuscitation is critical for treating a hypotensive patient. Although the pressure bag was indicated as the standard technique for fluid delivery by 55% of the survey recipients, the overall satisfaction with it is suspect. The survey indicated that most of the respondents believe using pressure bags is cumbersome (with 91% reporting the need to inflate the bag more than once), associated with concerns for air emboli (79% strongly agreed or agreed with potential risk), and difficult to deliver a rapid bolus when used with a small gauge catheter (83% strongly agreed or agreed with this challenge). Furthermore, the survey indicated that complex and slow set up and getting fluids in quickly are significant challenges for emergency nurses, with 32% and 42%, respectively, reporting it as the most significant challenge associated with the administration of rapid fluids. Taken together, it appears that, while pressure bags are commonly used to deliver rapid fluid boluses, they leave much to be desired. These sentiments are echoed by clinicians interviewed in this video about existing fluid administration methods:
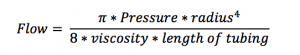
The subjective concerns of emergency nurses appear well justified. The flow of fluids through an IV catheter can be described by Poiseuille’s Law, which states that the flow can be represented by the following formula:
Looking closer, the pressure gradient is only one factor in determining how quickly fluid can be delivered. In fact, fluctuating the other factors such as the length and diameter of the catheter can lead to a 10-fold difference in flow rates (158 – 1428 ml/min).1 In other words, the time to deliver a fluid bolus via pressure bag can be quite variable. In fact, in one study, the amount of time to infuse 500 mL of liquid using a 20g central venous catheter via a pressure bag inflated to 300mm Hg could be as long as 18 minutes.2
When all things are equal (type of fluid, length and radius of tubing), applying additional pressure will certainly increase the flow rates. However, the pressure gradient must be maintained to ensure consistent flow rates. As a bag of fluid is infused and the volume of the bag decreases, the pressure bag needs to be consistently re-inflated to ensure pressure maintains at 300 mm Hg. In a study comparing a rapid infuser to pressure bag, the authors observed significantly longer infusion time associated with pressure bags.3 The authors attributed the increased time partially to the additional time needed to re-inflate the bag to maintain adequate pressure. Clinically, unless there’s a dedicated person monitoring and re-inflating the pressure cuff, it’s likely that infusion time will be further prolonged as the pressure gradient decreases. In a study evaluating different methods of rapidly delivering fluid in a prehospital setting, the use of a pressure cuff inflated to 200 mmHg initially without reinflation generated rapid flow, but the rate trailed off to nearly identical to gravity flow after 600 mL of a 1L bag was infused.4
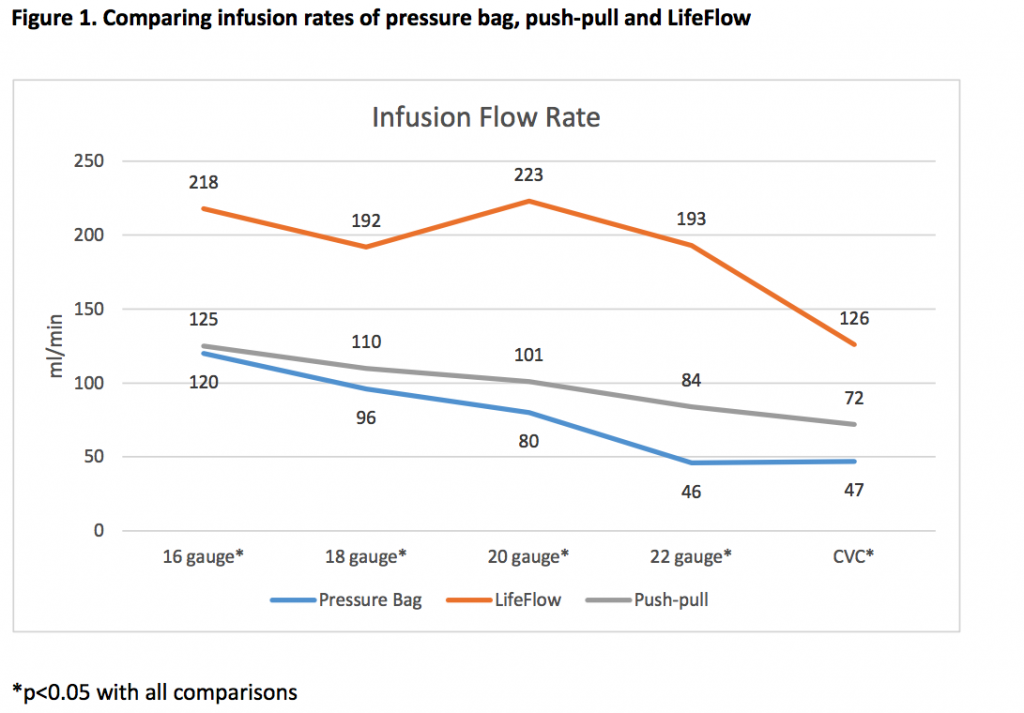
Furthermore, flow rates when using pressure bags are extremely sensitive to catheter diameter, where changes from 16g to 22g catheters consistently led to a 3-fold decrease in flow rates.5-7 Clinically, it’s rare to have the luxury of choosing from multiple available catheters and placing a new line may waste precious minutes while the patient is hypotensive. Unfortunately, large bore catheters are not routinely used. As observed in an international cross sectional study, 20-22g peripheral catheters are the most commonly used size in North America (3887 of 5258, 74%).8 Using these catheters, flow rates via pressure bags range from 46-150 ml/min, with the faster rates assuming a provider is constantly reinflating the bag.7,9,10 Lastly, if more than 1 liter needs to be infused, the take-down time to deflate and reinflate the pressure bag can take over 90 seconds.3
Lastly, while the reported incidence of air embolisms from pressure bags is low, there are numerous reports of fatal and near-fatal cases associated with their use.11-16 Venous air embolism can occur when a pressure gradient favors the entry of gas into the blood circulation. As little as 100-300 ml of air introduced to the circulatory system could be fatal.17 In each of the cases of air embolism reported, the use of pressure bags facilitated an environment which allowed for the possibility of intravascular air entrainment. The authors of the cases all agreed that high-level clinical vigilance and recognition must be employed when using pressure bags for fluid delivery. In some cases, authors also recommend the use of in-line air filters. While in-line filters can decrease the risk of air emboli, this risk reduction is limited by the capacity of the air filter, with most filters holding less than 3 mL of air. Furthermore, in-line air filters may also impede fluid flow and increase complexity and time of set up.
So, pressure bags typically are slow, particularly with small catheter diameters, and less effective without constant reinflation. They also require significant time for takedown and set-up and are sometimes associated with air embolisms. But what alternative do we have?
Based on the survey described above, a new device is sorely needed. Nearly all the ER nurses surveyed (52 of 53) agreed that a fluid bolus device that could reduce the complexity and stress in an emergency situation would be very helpful. LifeFlow® is a new handheld device for rapid, controlled delivery of a fluid bolus. It is quick and easy to set up and operated by one person. In a study at Yale New Haven Children’s Hospital, LifeFlow was shown to reduce perceived fluid resuscitation task load and complexity compared to pressure bag and push-pull.18 Also, in contrast to pressure bags, LifeFlow is designed to minimize the possibility of the user inadvertently administering air to the patient. In a speed comparison of pressure bag vs. LifeFlow to infuse 1L of IV fluid through a variety of catheters, LifeFlow was consistently faster.7,19 Furthermore, the flow rates were not nearly as susceptible to small catheter diameter. As the catheter sized changed from 16 to 22, flow rates fluctuated minimally from 192ml/min to 223 ml/min. This was in contrast to a pressure bag, where flow rates ranged from 46 to 120 ml/min (Figure 1).
Before reaching for the pressure bag next time you are confronted with a patient in shock or hypotension, consider that every minute counts. There are better methods for rapid fluid delivery. Either LifeFlow or push-pull will enable you to deliver a fluid bolus faster than a pressure bag. However, LifeFlow offers ease of use and decreased contamination risk. There IS a better option.
Interested in learning more about rapid, controlled delivery of a fluid bolus with LifeFlow? Contact us.
- Millikan JS, Cain TL, Hansbrough J. Rapid volume replacement for hypovolemic shock: a comparison of techniques and equipment. J Trauma. 1984;24:428-431.
- Kamata M, Walia H, Hakim M, Tumin D, Tobias JD. An In Vitro Assessment of the Efficacy of Various IV Cannulas for the Rapid IV Fluid Administration. Pediatr Crit Care Med. 2017;18:e224- e228.
- Iserson KV, Criss E. Combined effect of catheter and tubing size on fluid flow. Am J Emerg Med. 1986;4:238-240.
- Rottman SJ, Larmon B, Manix T. Rapid volume infusion in prehospital care. Prehosp Disaster Med. 1990;5:225-229; discussion 229-230.
- Khoyratty SI, Gajendragadkar PR, Polisetty K, Ward S, Skinner T, Gajendragadkar PR. Flow rates through intravenous access devices: an in vitro study. J Clin Anesth. 2016;31:101-105.
- Dula DJ, Muller HA, Donovan JW. Flow rate variance of commonly used IV infusion techniques. J Trauma. 1981;21:480-482.
- Robertson G, Lane A, Piehl M, Whitefill T, Spangler H. Comparison of a novel rapid fluid delivery device to traditional methods. https://410medical.com/wp-content/uploads/2018/03/Infusion- Rate-Comparison-of-LifeFlow-to-Traditional-Methods.pdf. Accessed 2018, September 18.
- Alexandrou E, Ray-Barruel G, Carr PJ, Frost SA, Inwood S, Higgins N, et al. Use of Short Peripheral Intravenous Catheters: Characteristics, Management, and Outcomes Worldwide. J Hosp Med. 2018;13.
- Reddick AD, Ronald J, Morrison WG. Intravenous fluid resuscitation: was Poiseuille right? Emerg Med J. 2011;28:201-202.
- Hu MH, Chan WH, Chen YC, Cherng CH, Lin CK, Tsai CS, et al. Effect of External Pressure and Catheter Gauge on Flow Rate, Kinetic Energy, and Endothelial Injury During Intravenous Fluid Administration in a Rabbit Model. Shock. 2016;45:98-103.
- Shamim F, Abbasi S. Fatal vascular air embolism during fluid resuscitation as a complication of pressure infuser bag. J Emerg Trauma Shock. 2016;9:46-47.
- Adinarayanan S, Ira B, Priya G. Massive air embolism through a peripheral venous cannula. British Journal of Anaesthesia. 2012;109.
- Bakan M, Topuz U, Esen A, Basaranoglu G, Ozturk E. Inadvertent venous air embolism during cesarean section: collapsible intravenous fluid bags without self-sealing outlet have risks. Case report. Braz J Anesthesiol. 2013;63:362-365.
- Suwanpratheep A, Siriussawakul A. Inadvertent venous air embolism from pressure infuser bag confirmed by transophageal echocardiography. J Anesth Clinic Res. 2011;2.
- Pant D, Narani KK, Sood J. Significant air embolism: A possibility even with collapsible intravenous fluid containers when used with rapid infuser system. Indian J Anaesth. 2010;54:49- 51.
- Gray AJ, Glover P. Air emboli with Haemaccel(R). Anaesthesia. 1999;54:790-792.
- Palmon SC, Moore LE, Lundberg J, Toung T. Venous air embolism: a review. J Clin Anesth.1997;9:251-257.
- Kline M, Crispino L, Bhatnagar A, Panchal RA, Auerbach M. A Randomized Single-BlindedSimulation-Based Trial of a Novel Method for Fluid Administration to a Septic Infant. Pediatr Emerg Care. 2018.
- Brooks EA, Piehl M. Potential mortality and cost reduction in adult severe sepsis and septic shock through the use of an innovative fluid delivery device. Open Access Emerg Med. 2018;10:165-170.

