
In many critical care situations, early, rapid fluid administration is vital to patient survival and improved outcomes. The nature of rapid delivery of fluids via a vascular line may create the opportunity for air to be inadvertently introduced into the vascular system. This clinical phenomenon is known as Vascular Air Embolism, or VAE. VAEs are defined as blood vessel blockages caused by one or more bubbles of air in the circulatory system, which may result in serious injury or death.1,2 A common cause of VAE is an access point between the vascular system and ambient air, coupled with a pressure gradient that drives the entry of air into the vascular system.2 Because the severity of sequalae from VAE is dependent on rate and volume of air infusion, the risk of VAE with rapid fluid administration is likely to be even higher than would be seen with standard infusion.
Because VAEs are hospital-acquired, preventable events, the Centers for Medicare and Medicaid Services (CMS) has deemed VAEs “never events” and will not reimburse institutions for its medical management.3 While the incidence of VAEs is quite low, volumes as low as 50ml have been reported to be lethal.4 Mortality rates have been reported to be as high as 48-80%.5 As IV bags have been shown to contain a volume of ~60ml of air,6 this provides an opportunity for air to enter with inappropriate handling. In one reported case, a 56-year-old male experienced sudden-onset bradycardia, hypotension, and hypoxia when it was discovered that that air was present in the IV tubing and saline bag. The healthcare team realized the bag of saline had been removed for the addition of mannitol and was then reconnected. Enough air had entered the bag that pressure inside the bag was greater than atmospheric pressure, and air had continued to flow after the fluid had emptied.7
In a variety of clinical treatment areas, efforts have been made to avoid the opportunity for VAEs to develop. Some nurses use a technique called “burping” to release any air in the IV bag prior to connection, but this is not well documented in standard training and practice. Additionally, the process of removing and re-inserting the spike to de-air the bag can result in contamination, which goes against infection prevention practices.
Another more reliable option, particularly in the setting of rapid fluid delivery, is to use a closed-system device. LifeFlow® is one such device, with built-in safety features (see Fig. 1) designed to warn and protect against air introduction to intravenous lines.
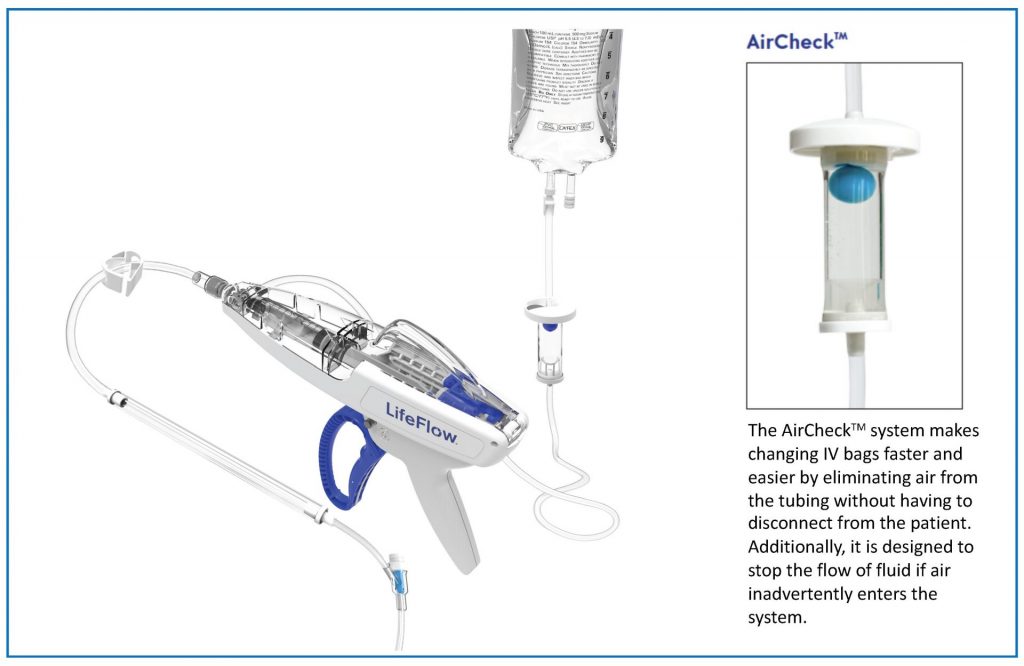
Fig 1. LifeFlow Infuser with AirCheck™ system
Hypovolemic patients are particularly susceptible to VAEs due to the presumed low central venous pressure, high rate of flow needed, and urgency of the situation.8 Pressure bags are often the go-to method for rapid volume infusion in critical care situations due to their low cost and established use. However, data shows that use of pressure bags can provide entry point for air.7 Pressure bags lack safety features to prevent air or alert providers about air having entered the vasculature, and an embolism may not be detected until the patient’s condition begins to deteriorate.
Additionally, studies have shown that pressure bags have a long infusion time when compared to a rapid infuser. Specifically in comparison to LifeFlow, pressure bags take 3x longer to deliver a bolus.9 For patients in shock, every minute matters in fluid resuscitation to reverse hypotension and restore perfusion.10 As medical devices evolve to include necessary safety features, it’s important that we reconsider our routine use of pressure bags and replace them with safer, more efficient options to avoid VAEs without sacrificing time-to-treatment.
Want to learn more about LifeFlow? Contact us.
- https://www.healthline.com/health/air-embolism
- Int J Crit Illn Inj Sci. 2013 Jan-Mar; 3(1): 73–76.
- Department of Health and Human Services. Letter to State Medicaid Directors. 31 Jul 2008. p 5. https://downloads.cms.gov/cmsgov/archived-downloads/smdl/downloads/smd073108.pdf
- Malki, et al. Em Resident. 9 Oct 2020. https://www.emra.org/emresident/article/venous-air-embolism/
- Shaikh, et al. J Emerg Trauma Shock. 2009 Sep-Dec; 2(3): 180–185.
- Munsun ES. Air from IV Bags May Pose Danger; Venous Embolism Comes from Many Causes. APSF Newsletter. Volume 8, No. 2 • Summer 1993.
- Cook LS. Infusion-Related Air Embolism. Jour of Infusion Nursing. Jan-Feb 2013;36(1):26-36.
- Natal, et al. Venous Air Embolism. Theheart.org, Medscape. 30 Dec 2017. https://emedicine.medscape.com/article/761367-print
- Robertson, G., Lane, A., Piehl, M., Whitfill, T., Spangler, H. (2018) Comparison of a novel rapid fluid delivery device to traditional methods. [White paper]. Data in Table 1.
- Maheshwari K, et al. (2018) The relationship between ICU hypotension and in-hospital mortality and morbidity in septic patients. Intens Care Med. Jun;44(6):857-867.

