Pediatric septic shock affects over 75,000 children annually in the United States. Although many of these cases are reversible with rapid fluid resuscitation, the mortality rate ranges from 9-25% overall and is as high as 50% in certain high-risk populations.1 Rapid fluid administration is a key intervention for early shock reversal and the prevention of complications.
American College of Critical Care Medicine (ACCM) guidelines recommend giving a rapid fluid bolus of 20mL/kg within five minutes followed by an assessment of perfusion and cardiorespiratory status between each additional bolus.2 However, effective fluid resuscitation in pediatric patients is often complicated by difficult intravenous (IV) access. The dehydrated veins of a patient in shock are more difficult for nurses to identify and insert a large-gauge IV catheter. As a result, many patients who need fluids have only a single small-bore catheter in place.
Smaller catheters are more prone to infiltration during rapid fluid administration. In addition, traditional rapid infusion methods often perform poorly with small-gauge catheters.3-5 This delays essential fluid administration for reversing shock and preventing complications.
The following case from a large children’s hospital in Colorado highlights the positive impact of using a handheld rapid infuser to quickly administer multiple fluid boluses to a patient experiencing septic shock with limited IV access.
Case Presentation & Challenges
A 14-year-old male patient arrived in the emergency room with a chief complaint of a cough and two days of fever. The patient’s medical history included cerebral palsy and multiple pneumonias with hypoxia. Notably, nurses had an “extremely difficult” time obtaining IV access in this patient upon his arrival.
Assessment of the patient’s vital signs revealed a blood pressure of 70/40 mmHg and an elevated heart rate of 136, indicating shock. The patient’s capillary refill was also slightly delayed at 3-4 seconds. His appearance was pale with mottled skin and waning mentation.
Management
Recognizing the patient’s state of decompensated shock, the medical team immediately ordered the start of rapid fluid resuscitation. Using the LifeFlow® rapid infuser, nurses administered three 880 mL normal saline boluses (total of 2640 mL). Each bolus was infused over four to five minutes through a 24-gauge IV in the patient’s wrist.
Following the second bolus, an assessment of the patient revealed improving vital signs, including an increase in blood pressure and a decrease in heart rate. The patient also exhibited decreased anxiety and began to recognize his surroundings once again.
After the three fluid boluses were administered, the nurses successfully placed a 20 gauge IV in the patient’s AC. He was then started on norepinephrine and transferred to the pediatric ICU for further care.
Discussion
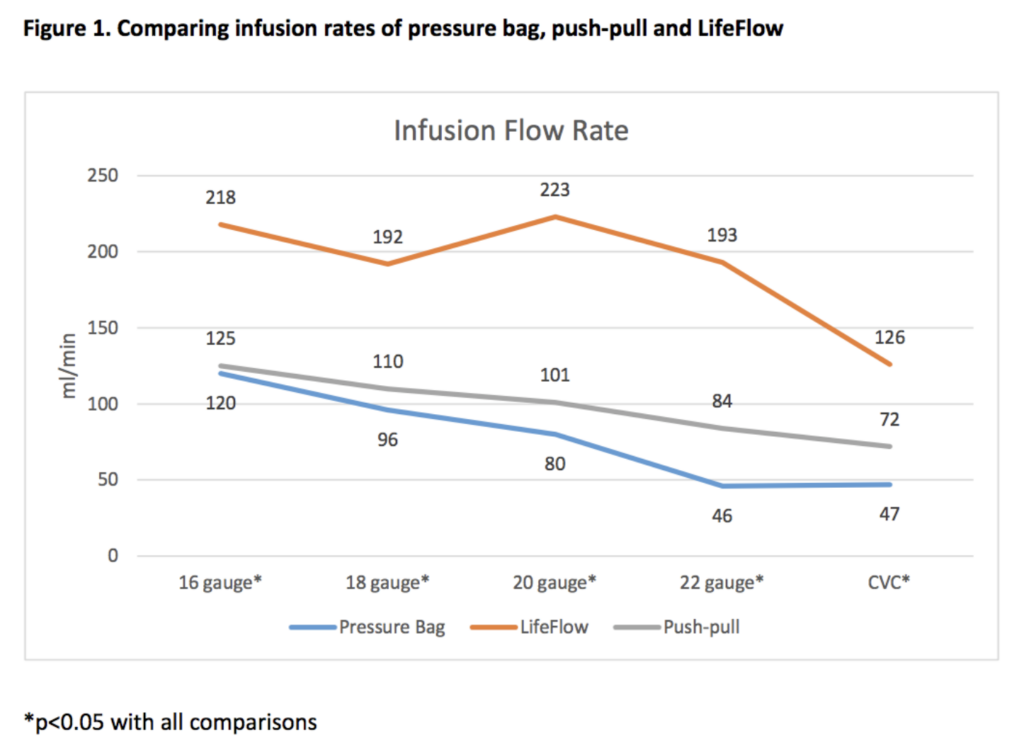
Patients in septic shock require immediate intervention, including rapid fluid resuscitation. In pediatric patients, this workflow is often complicated by difficult IV access. Administering a bolus according to ACCM guidelines using traditional rapid infusion methods becomes more difficult as the catheter diameter shrinks. As shown in Figure 1, the LifeFlow device’s flow rate outperforms traditional methods across all sizes of catheters.4
In this case, providers administered fluids using the LifeFlow handheld infuser due to the need for rapid fluid replacement and limited IV access. The device allowed the team to safely deliver fluids according to ACCM guidelines while preserving a delicate yet important IV site. Nurses who administered the fluids highlighted the device’s Force Reducer™ , which decreases pressure in the system and reduces the amount of effort required from the user. The team also noted the ability to “feel” the status of the IV via the device’s handle, allowing them to protect the site and adjust the rate of fluid administration based on the patient’s response.
When pediatric patients in septic shock need emergent fluid replacement, small-gauge IVs and difficult IV access often delay care. However, efficient fluid resuscitation is essential to decreasing mortality and preventing complications. The LifeFlow device’s excellent flow rate with IV catheters of all sizes allows providers to safely and rapidly administer fluids when every minute matters.
1. Workman, J. K., Bailly, D. K., Reeder, R. W., Dalton, H. J., Berg, R. A., Shanley, T. P., Newth, C. J. L., Pollack, M. M., Wessel, D., Carcillo, J., Harrison, R., Dean, J. M., Meert, K. L., & Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Collaborative Pediatric Critical Care Research Network (CPCCRN) (2020). Risk Factors for Mortality in Refractory Pediatric Septic Shock Supported with Extracorporeal Life Support. ASAIO journal (American Society for Artificial Internal Organs : 1992), 66(10), 1152–1160. https://doi.org/10.1097/MAT.0000000000001147
2. Stoner, M. J., Goodman, D. G., Cohen, D. M., Fernandez, S. A., & Hall, M. W. (2007). Rapid fluid resuscitation in pediatrics: testing the American College of Critical Care Medicine guideline. Annals of emergency medicine, 50(5), 601–607. https://doi.org/10.1016/j.annemergmed.2007.06.482
3. Dula DJ, Muller HA, Donovan JW. Flow rate variance of commonly used IV infusion techniques. J Trauma. 1981;21:480-482.
4. Robertson G, Lane A, Piehl M, Whitefill T, Spangler H. Comparison of a novel rapid fluid delivery device to traditional methods. https://410medical.com/wp-content/uploads/2018/03/Infusion-Rate-Comparison-of-LifeFlow-to-Traditional-Methods.pdf. Accessed 2018, September 18.
5. Iserson KV, Criss E. Combined effect of catheter and tubing size on fluid flow. Am J Emerg Med. 1986;4:238-240.