In Part 2 of this series, we discussed a 30kg 10-year old septic patient who needed three 20ml/kg boluses of fluid to quickly restore adequate perfusion. If we had used a 30mL syringe to administer the fluid, it would have required up to 60 separate syringes using the disconnect-reconnect method, or 60 strokes of a syringe plunger using the push-pull method. What if the risk of causing a CLABSI increased dramatically with each syringe or each stroke? There is a growing body of research that suggests we increase the risk of bacterial contamination when using these techniques.
More than 250,000 catheter-related bloodstream infections (CLABSIs) occur annually in the United States1, resulting in significant morbidity and mortality.2,3 One CLABSI can result in excess hospital costs of $70,0004 and subjects patients to a two-fold increase in the risk of death.5 The risk of a CLABSI increases with each step of syringe-based fluid administration: syringe preparation, catheter hub access, and pulling and depressing the syringe plunger. Several studies have highlighted the risk of bacterial transfer from contaminated gloves to the syringe plunger and subsequently into the fluid delivered to the patient.6,7 In a study evaluating conventional syringes inoculated with the Bacillus species of bacteria, two or more strokes of the plunger inevitably led to the transport of the contaminant into the sterile chamber of the syringe.7 Furthermore, a direct correlation between the number of aspirations and the degree of contamination was observed.6 The pathway of a syringe hub contamination is clearly demonstrated in this video, which shows how a contaminant can travel from a provider’s hand into the syringe and ultimately into the patient.
Thinking back to the last time you used a syringe to administer fluid, can you be sure you never touched the stem of the plunger as you pulled or pushed the syringe? When we’re in an emergency situation where a patient is crashing and needs fluids ASAP, we’re doing everything we can to get fluids in quickly, and this often means we repeatedly grab the syringe plunger or inadvertently contaminate the sterile end a syringe or stopcock. It just happens. Particularly as the work to cycle the syringe 20, 40, or 60 times creates more and more fatigue as we discussed in Part 2 of this series.
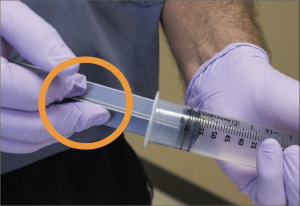
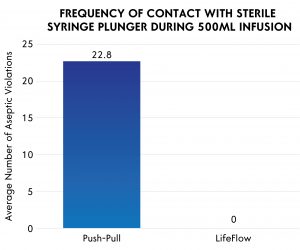
A recent study evaluated aseptic technique during fluid administration comparing the push-pull technique and Lifeflow®, a new rapid fluid bolus device .8 In a simulated patient care environment, providers were observed delivering fluid according to their usual clinical practice. When the push-pull technique was used, every user in the study had multiple plunger violations (mean = 22.8 violations per patient). In contrast, zero violations were noted when the Lifeflow device was used. The investigators also performed a benchtop experiment which clearly observed small particle contaminants crossing into the syringe during the push-pull technique. Similar findings have been observed in other studies.6
Is the disconnect-reconnect method any better with regards to contamination risk? Unfortunately, no. A recent study found that manually filling and emptying a syringe, even for a single flush, results in more than double the number of infections compared to using syringes pre-filled by the manufacturer.9 If a provider followed perfect aseptic technique while filling, dispensing, and connecting each syringe, the risk of contamination would be low. But when a patient is critically ill, how many of us actually “scrub the hub” for 30, or even 15, seconds? And each time a new syringe is connected to the IV tubing presents a new opportunity for contamination. Even wearing disposable gloves may not prevent contamination. Disposable gloves are not sterile and previous studies have shown contamination in over 80% of gloves, even before they are removed from the box.10,11 Perfect aseptic technique almost always takes a back seat to providing effective resuscitation.
This 3-part series evaluated fluid administration techniques routinely used on critically ill pediatric patients. Disconnect-reconnect and push-pull, the most commonly used techniques, also carry serious risks, such as CLABSIs. The American Society of Anesthesiologists and the American Association of Nurse Anesthetists recently published guidelines recommending a single syringe be used only one time.12,13 Though the push-pull and disconnect-reconnect methods continue to be the most frequently used techniques for rapid fluid resuscitation in the pediatric ICU, ED and OR settings, we owe it to our patients to find better and safer methods for rapid fluid resuscitation.
- O’Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO, Lipsett PA, Masur H, Mermel LA, Pearson ML, Raad, II, Randolph AG, Rupp ME, Saint S, Healthcare Infection Control Practices Advisory C. Summary of recommendations: Guidelines for the Prevention of Intravascular Catheter-related Infections. Clin Infect Dis. 2011;52:1087-1099.
- Maki DG, Kluger DM, Crnich CJ. The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo Clin Proc. 2006;81:1159-1171.
- Magill SS, Edwards JR, Bamberg W, Beldavs ZG, Dumyati G, Kainer MA, Lynfield R, Maloney M, McAllister-Hollod L, Nadle J, Ray SM, Thompson DL, Wilson LE, Fridkin SK, Emerging Infections Program Healthcare-Associated I, Antimicrobial Use Prevalence Survey T. Multistate point- prevalence survey of health care-associated infections. N Engl J Med. 2014;370:1198-1208.
- Eliminating CLABSI, A National Patient Safety Imperative: Final Report Companion https://www.ahrq.gov/professionals/quality-patient-safety/cusp/clabsi-final- companion/clabsicomp4c.html. Accessed Aug 15, 2018.
- Stevens V, Geiger K, Concannon C, Nelson RE, Brown J, Dumyati G. Inpatient costs, mortality and 30-day re-admission in patients with central-line-associated bloodstream infections. Clin Microbiol Infect. 2014;20:O318-324.
- Olivier LC, Kendoff D, Wolfhard U, Nast-Kolb D, Nazif Yazici M, Esche Modified syringe design prevents plunger-related contamination–results of contamination and flow-rate tests. J Hosp Infect. 2003;53:140-143.
- Blogg CE, Ramsay MA, Jarvis JD. Infection hazard from syringes. Br J Anaesth. 1974;46:260-262.
- Spangler H, Lane A, Piehl M, Robertson G. Improving septic technique during the treatment of pediatric septic shock: A comparison of two rapid fluid delivery methods. Journal of Infusion Nursing. 2018: Accepted for publication: In Press.
- Bertoglio S, Rezzo R, Merlo FD, Solari N, Palombo D, Vassallo F, Beltramini S, DeMaria A. Pre- filled normal saline syringes to reduce totally implantable venous access device-associated bloodstream infection: a single institution pilot study. J Hosp Infect. 2013;84:85-88.
- Assadian O, Leaper DJ, Kramer A, Ousey Can the design of glove dispensing boxes influence glove contamination? J Hosp Infect. 2016;94:259-262.
- Hughes KA, Cornwall J, Theis JC, Brooks HJ. Bacterial contamination of unused, disposable non- sterile gloves on a hospital orthopaedic ward. Australas Med J. 2013;6:331-338.
- ASA Committee on Occupational Health Rask Force on Infection Control. Recommendations for Infection Control for the Practice of Anesthesiology (Third Edition). https://www.asahq.org/standards-and-guidelines/resources-from-asa-committees#ic. Accessed Aug 15, 2018.
- American Association of Nurse Anesthetists. Safe Injection Guidelines for Needle and Syringe Use. https://www.asahq.org/standards-and-guidelines/resources-from-asa-committees#ic Accessed Aug 15, 2018.

